Best Gastroenterology Treatments: A Comprehensive Guide
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. This includes the gastrointestinal (GI) tract, which spans from the mouth to the anus, as well as organs like the liver, pancreas, and gallbladder. With millions of people worldwide suffering from GI conditions—ranging from acid reflux to more serious diseases like Crohn’s or colorectal cancer—the need for effective gastroenterology treatments is greater than ever.
In recent years, advances in diagnostic tools, minimally invasive procedures, and personalized medicine have significantly improved outcomes. Here’s a comprehensive look at the best gastroenterology treatments available today.
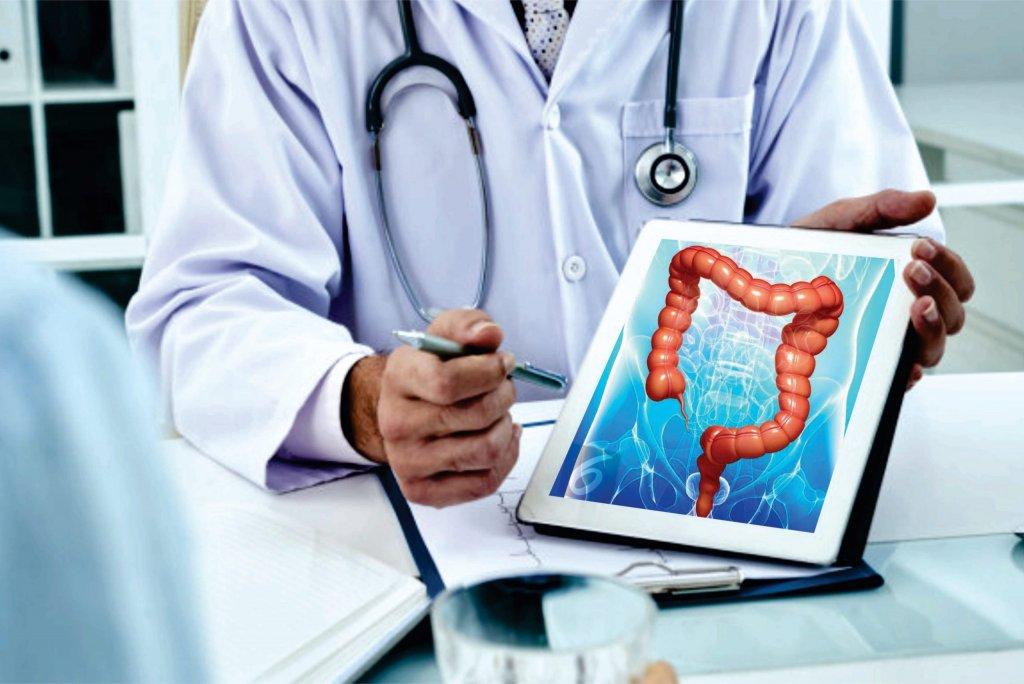
1. Endoscopy and Colonoscopy: Gold Standards for Diagnosis and Treatment
Endoscopy and colonoscopy are the cornerstone diagnostic tools in gastroenterology.
- Endoscopy allows doctors to view the upper GI tract (esophagus, stomach, and duodenum) using a flexible tube with a camera. It is essential for diagnosing ulcers, gastritis, and early signs of esophageal or stomach cancer.
- Colonoscopy is used to examine the colon and rectum. It is crucial for detecting polyps, colorectal cancer, and inflammatory bowel diseases like Crohn’s and ulcerative colitis.
Both procedures can be therapeutic as well—removing polyps, controlling bleeding, or dilating strictures during the same session.
2. Pharmacological Treatments
Medication remains the first line of treatment for many GI disorders:
- Proton Pump Inhibitors (PPIs) are widely used for acid reflux, GERD, and peptic ulcers.
- Antibiotics are essential for treating Helicobacter pylori infections, which can cause ulcers and increase stomach cancer risk.
- Aminosalicylates and immunomodulators are used to manage inflammatory bowel disease (IBD).
- Biologics, such as anti-TNF agents (e.g., infliximab, adalimumab), have revolutionized treatment for Crohn’s and ulcerative colitis, providing relief when conventional drugs fail.
- Laxatives and antispasmodics help manage symptoms of IBS (Irritable Bowel Syndrome).
Personalized medicine—where genetic and microbiome profiles help guide drug selection—is an emerging field that promises even more targeted and effective therapies.
3. Minimally Invasive Procedures
Minimally invasive techniques reduce recovery time, pain, and risk of complications.
- Endoscopic Ultrasound (EUS) combines endoscopy and ultrasound to evaluate organs near the GI tract, especially the pancreas and bile ducts.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) is used to diagnose and treat bile duct and pancreatic duct problems, including gallstones and tumors.
- Capsule Endoscopy, a swallowable camera pill, allows for non-invasive imaging of the small intestine—an area previously hard to reach.
These techniques are increasingly replacing open surgeries for many patients.
4. Surgical Interventions
In cases where medication or endoscopy isn’t sufficient, surgery may be necessary.
- Laparoscopic surgery offers a less invasive alternative to traditional open surgery for conditions like gallstones, hernias, or colorectal cancer.
- Bariatric surgery, although primarily for obesity, also benefits GI health by improving reflux and liver disease.
- Bowel resection may be required in severe cases of IBD or cancer.
Surgeons now use robotic-assisted techniques for greater precision and faster recovery.
5. Liver Disease Management
The liver is a vital organ in digestion, and its diseases require specialized treatments:
- Antiviral therapies for hepatitis B and C have transformed liver disease outcomes, with hepatitis C now considered curable in most cases.
- Lifestyle changes, such as diet and exercise, are first-line treatments for fatty liver disease (NAFLD and NASH).
- Liver transplantation remains the ultimate solution for end-stage liver disease, with improved success rates thanks to better immunosuppressive drugs and surgical techniques.
6. Nutritional and Lifestyle Counseling
A holistic approach is essential in gastroenterology. Diet and lifestyle play a major role in both prevention and management.
- Dietary changes, such as a low-FODMAP diet for IBS or gluten-free diet for celiac disease, are central to symptom control.
- Behavioral therapy and stress management are also effective for conditions like IBS, where psychological factors influence gut function.
Gastroenterologists increasingly collaborate with dietitians, psychologists, and primary care providers to offer integrated care.
7. Cutting-Edge Therapies and Future Outlook
The future of gastroenterology is exciting, with several promising developments:
- Microbiome therapies (e.g., fecal microbiota transplantation) are being explored for a variety of conditions, including IBD and C. difficile infections.
- Artificial intelligence (AI) is being used to enhance endoscopic imaging and early cancer detection.
- Gene therapy and stem cell therapy hold potential for treating previously incurable diseases.
As research continues, we can expect even more precise, effective, and less invasive treatments in the coming years.
Conclusion
The field of gastroenterology has evolved rapidly, offering a wide range of effective treatments for digestive disorders. From simple dietary interventions to advanced biologics and robotic surgery, today’s gastroenterologists are equipped with tools to diagnose, treat, and even cure many conditions that were once debilitating or fatal. With continued innovation and a growing focus on personalized care, the future of digestive health looks brighter than ever.