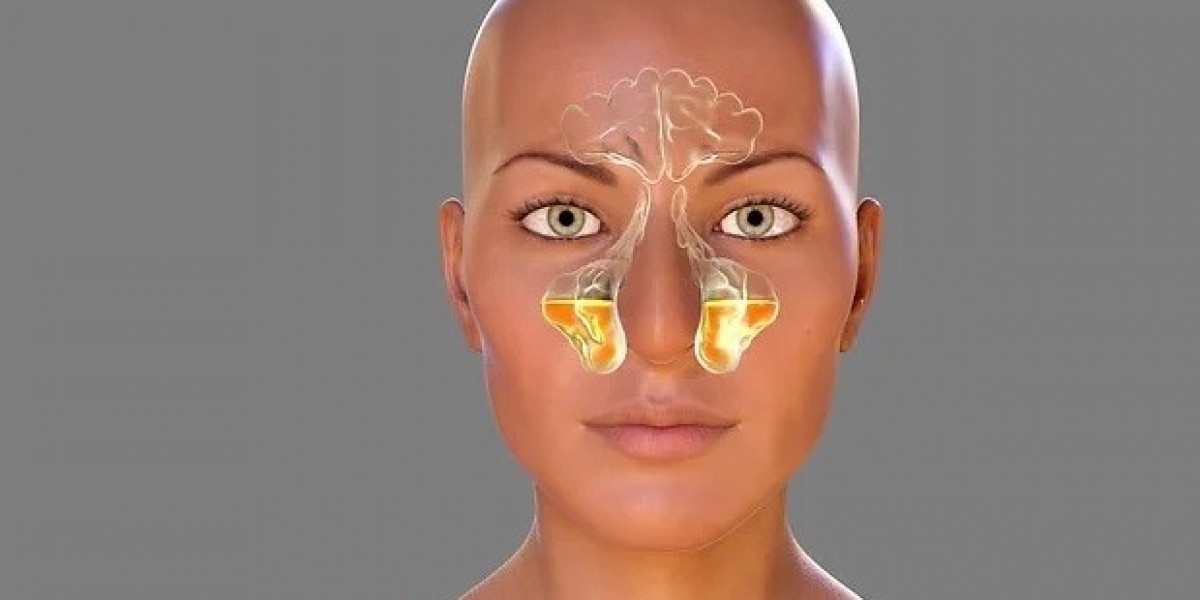
Most fungal sinusitis cases are non-invasive, and they limit to the nasal cavity (in the nose) and sinuses. However, if immunity gets compromised, a non-invasive infection can transform into an invasive disease. The fungus that infects the skin lining of the nose and sinuses will move into the deeper tissues, thus making it more dangerous. This type of infection that spreads into the tissues is invasive fungal sinusitis. In some we see a rare symptom where the disease is untreated or incorrectly treated, the infection can also spread from tissues to facial skin. So, in non-invasive fungal sinusitis, the fungus only lives in the sinus cavity. But, in invasive fungal infection, the fungus lives in tissues. Sometimes the patient could be having both invasive and non-invasive infections at different places. For example, the patient could have a non-invasive fungal infection in the nose or maxillary sinus and an invasive fungal infection in other sinuses like the sphenoid sinus. The ENT doctor must carefully check for both.
Difference between Granulomatous and Non-granulomatous invasive fungal sinusitis
Granulomas are well-developed immune system cells present around the fungus and try to fight the fungal infection. If these granulomas are present around the fungal infection, it will be granulomatous fungal sinusitis. Else, it is called non-granulomatous fungal sinusitis. Given the right combination of medicines, recovery is quicker for a granulomatous fungal sinus infection than for a non-granulomatous fungal sinus infection.
How is invasive fungal sinusitis different from fulminant fungal sinusitis?
Mucormycosis and Aspergillosis fungal sinusitis, commonly known as black and white fungus respectively, are invasive fungal sinusitis but come under a subtype called fulminant. Although fulminant comes under invasive, when we say invasive fungal sinusitis we always refer to non-fulminant invasive fungal sinusitis. Immunity is more compromised in fulminant than an invasive fungal infection. In these fulminant infections, the spread is faster, and the infection can double up in hours. Whereas Invasive fungal sinusitis far more time to double up. This characteristic makes them so distinctive that a doctor can easily differentiate these two types of fungal sinus infections based on the timeline of the symptoms, although both infections have similar symptoms. The differentiating feature of fulminant infection is that the disease spreads to the blood vessels.
The mortality rate is higher in the fulminant fungal infection as it can spread faster than invasive fungal sinusitis as fulminant can reach the brain within a few weeks if not treated. Thankfully it will take years for the invasive fungal sinusitis to do the same, giving us time to deal with it. When treated early, the mortality rate of fulminant fungal sinusitis is 30%, but if treated, the mortality rate is almost zero for invasive fungal sinusitis.
The type of fungal infection depends solely on immunity. Low immunity means non-invasive type, very low means invasive type, very very low means fulminant type.
Invasive fungal sinusitis symptoms
The infection can spread from the sinuses to other parts of nearby sinuses, hence here are the invasive fungal sinusitis symptoms.
• Pain and/or swelling in the eye, nose, teeth, or cheek
• Vision disturbances – double vision or diminishing vision
• Loosening of the teeth when the infection spreads to the jaw bone
• Loss of sensation in the cheek
• Swelling of the face if it spreads to the skin – a rare condition
• When it spreads to the brain, the body part controlled by that part of a particular brain area will be affected.
Example: In one of the invasive fungal sinusitis cases seen by Dr. K. R. Meghanadh, the left side of the brain that controls the right arm got invaded by the disease. The infection resulted in paralysis of the right arm.
Invasive fungal sinusitis symptoms and fulminant sinusitis symptoms are the same. Still, an ENT doctor can easily distinguish the symptoms as they progress slowly in invasive compared to fulminant infection in invasive fungal sinusitis.